When are cortisone shots appropriate? Evidence for rotator cuff tears/bursitis? Side effects/risks? Affect tendon integrity and contribute to tears/ruptures?
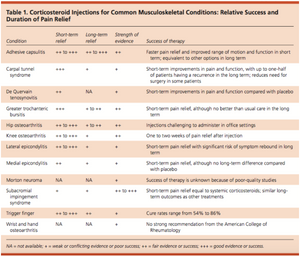
MSK Conditions
Adhesive Capsulitis
- Short term (8-16 week) improvements in pain and Range of Motion (ROM).
- Should recommend conservative treatment initially, adding oral or injected corticosteroids if there is not an adequate improvement in pain, ROM, or function.
- Consider subacromial corticosteroid injection before referring to manipulation under anesthesia because it poses less risk. Subacromial Impingement Syndrome
- Included rotator cuff syndrome, tendinitis, and bursitis.
- Corticosteroid injections provide a max of 4 weeks of pain relief.
- Intra-articular injections are no better than placebo; subacromial injections provide only minimal relief.
- Injections have similar to worse outcomes compared to conservative care.
- A combo of physical therapy and corticosteroid injections provides better pain relief at 6 weeks compared with physical therapy alone, but by 12 and 24 weeks there is no difference between treatments.
- Should recommend conservative therapies initially for the treatment of subacromial impingement syndrome. Patient preferences and duration of symptoms should also be considered; injections are more effective for those with symptoms of <12 weeks duration.
Lateral Epicondylitis
- In patients with symptoms up to 6 weeks in duration, corticosteroid injection provides pain relief for 4-6 weeks.
- Long-term outcomes indicate no benefit or symptom worsening.
- Recurrence rate 1 year after a single injection is >50%, compared with a 12% recurrence rate in those receiving placebo. Should warn patients of the high recurrence rate.
Medial epicondylitis
- Corticosteroid injection can provide short-term improvements in pain, although there is no long-term difference in outcomes between injection and placebo at 6 weeks to 1 year.
- Platelet-rich plasma (PRP) injection provides greater improvement in pain and function at 52 weeks compared with corticosteroid injection, although it is unclear whether this is clinically meaningful to patients.
Carpal Tunnel Syndrome
- Corticosteroid injections are beneficial in improving short-term outcomes.
- Patients who receive injection (as opposed to systemic corticosteroids) have significantly better symptom scores by 8 and 12 weeks.
- 2 injections provide no additional improvement compared with only 1 injection.
- Long-term → up to ½ have symptom recurrence.
- Need for surgery at 1 year is reduced with corticosteroid injection, but a significant number of patients (in the study, 75%) eventually undergo surgical treatment
De Quervain Tenosynovitis
- Corticosteroid injection is supported over splinting (this study was on pregnant and lactate women.)
- Improved pain and function at one week after corticosteroid injection (compared to placebo.)
- Injection alone results in improved outcomes compared with a combination of injection and splinting.
- Physician should consider injection. Referral for surgery may be considered if symptoms don’t resolve after injections.
Trigger Finger
- Cure rates after corticosteroid injection range from 54-86%
- Compared to placebo injection, corticosteroids results in less triggering and improved pain at 1 week, and these effects persist through 1 year
- Patients who underwent surgery had better outcomes at 6 months.
- Symptom relapse in: 12% who received 1 injection, 18% who received 2nd injection, and none who underwent surgery.
- Studies are limited by small sample size and short duration of follow-up.
- Corticosteroid injection should be offered for those seeking nonsurgical treatment option
Wrist/hand OA
- “No strong recommendation” for intra-articular corticosteroid injection.
- Best advised to refer patients to subspecialist if they desire this treatment.
Greater trochanteric bursitis
- Compared with analgesics and physical therapy, corticosteroid injections provide greater pain relief at rest and with activity at 6 weeks and 3 months, but no difference in pain or function at 6 months and 1 year.
- May consider injection for those who desire more prompt symptom resolution.
Hip OA
- Small double-blind study – corticosteroid vs placebo injections using an ultrasound-guided anterolateral approach → improvement in pain on walking at 2 and 4 weeks (corticosteroid group), but this improvement disappeared by 3 months.
- Fluoroscopically guided corticosteroid injections provide improvement in pain, stiffness, and physical function at 2 months.
- For patients who desire injection treatment, should consider orthopedic referral.
Knee OA
- Guidelines from the American College of Rheumatology conditionally recommend the use of intra-articular corticosteroid injections.
- In most studies – duration of pain relief is 1-2 weeks.
- Cochrane review – weak evidence for the use of corticosteroid injection.
Morton Neuroma
- Corticosteroid injection is considered a standard treatment.
- May consider corticosteroid injection, but should be advised there is no good-quality evidence to support it.
Appendix 1:

Foster ZJ, Voss TT, Hatch J, Frimodig A. Corticosteroid injections for common musculoskeletal conditions. American family physician. 2015;92(8): 694-699.
B Gialanella, P Prometti. Effects of corticosteroids injection in rotator cuff tears. Pain medicine. 2011; 12: 1559-1565
Objective: evaluate the effect of intraarticular injections of corticosteroids (triamcinolone) in patients with symptomatic rotator cuff tear (RCT).
60 patients with full-thickness rotator cuff tears, 3 groups of 20. All underwent rehab sessions. Outcome measures were pain (VAS) and shoulder functional status (Constant-Murley score), assessed at baseline, 3-months and 6-months follow-up. Pain also assessed at 1 month through telephone contact.
- Group 1 (TA1) – single intraarticular injection (40mg triamcinolone)
- Group 2 (TA2) – 2 injections (40mg triamcinolone) at 21-day interval
- Group 3 (Control) – control.Inclusion criteria:
- + Imaging diagnosis of full-thickness RCT
- Surgery not considered as 1st treatment of choice
- >75 years oldExclusion Criteria:
- Inflammatory rheumatic diseases
- History of fracture or operations around the shoulder region
- Neurological disease (that may lead to shoulder pain)
- Infections or tumours
- Hypersensitivity to TA
- Pregnancy
- Diabetes
- Coagulation diseases
- Intraarticular injections in the involved shoulder in the last 12 monthsMethods – intraarticular injection through a posterior approach and without local anesthesia. All patients underwent 15 sessions (20min each) of passive GH joint mobilization (taking into account the limit imposed by pain and cuff strengthening exercises. Patients were followed for 6 months.
Results – Pain - TA1 and TA2 significantly improved in activity pain and pain at night at all time points vs. baseline.
- TA1 significantly improved in rest pain at 1 and 3 months.
- Groups differed in pain at night score and activity pain at 1 and 3 months only. TA1 and TA2 did not differ in pain scoresResults – Functional Status
- TA1 and TA2 significantly improved in Total Constant-Murley and Constant-Murley ADLs score at all time points vs. baseline.
- No statistically significant difference among groups at any time in Constant-Murley scoresConclusion
- Intraarticular injection of TA improves pain relief in RCT for up to 3 months and additional injections after 21 days do not increase TA therapeutic effect
- Single instead of double dose is preferred. Single injections should be used when other conservative treatments fail or when rest or night pain increases (ie acute/inflammatory stages)
Other research
- Showed positive results in patients with RCT treated with combinations of rehab, anti-inflammatory agents, and local corticosteroid injections
- Improvement in pain relief, muscle strength and ROM in RCT patients treated with conservative treatment, including injections of lidocaine and dexamethasone sodium phosphate into the subacromial bursa.
- Pain relief in patients with RCT treated with corticosteroids but no significant difference in improvement of pain and efficacy between patients treaded with sodium hyaluronate versus dexamethasone.
- In supraspinatus tears, local corticosteroids resulted in some pain relief but did not improve ROM and painful arc and concluded that there was no objective evidence that local corticosteroids might improve the condition
Maman E, Yehuda C, Pritsch T, Morag G, Brosh T, Sharfman Z, et al. Deterimental effect of repeated and single subacromial corticosteroid injections on the intact and injured rotator cuff; a biomechanical and imaging study in rats. American journal of sports medicine. 2016; 44:1; 177-182.
Methods – 70 rats, 7 groups
Uninjured (no tear)
- Single saline injections (NS)
- Single methylprednisolone acetate (MTA) injection (ST)
- Triple MTA injections (ST3)Injured (unilateral supraspinatus injury)
- Single saline injections (NST)
- Triple saline injections (NST3)
- Single MTA injection (STT)
- Triple MTA injections (subacromial, repeated injections were administered weekly) (STT3)
Results
- Healthy rotator cuffs (RC) exposed to triple MTA injections had significantly decreased maximal load and stiffness compared with the control group.
- Injured RCs exposed to (1) steroid treatment had significantly lower maximal load compared with control at 3 weeks
- Greater tuberosity volume density and connectivity density were significantly lower in undamaged rats after triple MTA injection.
Corticosteroid Injection on intact RC
- Single MTA injection reduced the mean maximal load to failure (17.6%)
- Repeated MTA injections decreased the mean maximal load in the ST3 (triple MTA) group compared with the control group (32.1%)
- No significant differences between the ST and ST3 groups; however, slight decrease in the maximal load
Single vs. Triple corticosteroid injections on injured RC
- Single MTA injection reduced the mean max load to failure (22.7%)
- Triple MTA treatment reduced the mean maximal load (26.1%)Micro-CT analysis
- Significantly lower greater tuberosity volume density, connectivity density and trabecular number in undamaged RCs after triple MTA injections.
- Bone volume density and trabecular number were significantly lower in the ST3 group compared with the ST group.
- Connectivity density was significantly decreased in the ST3 group compared with both the NS and ST groups.
Conclusion
- Repeated doses of corticosteroids significantly weaken rat RC and negatively affected bone quality in addition to possibly causing deterioration of the osteotendinous junction.
Brinks A, Koes BW, VOlkers ACW, Verhaat JAN, Bierma-Seinstra SMA. Adverse effects of extra-articular corticosteroid injections: a systematic review. BMC Musculoskeletal disorders. 2010. 11;206
87 relevant studies (1956-2010); 44 case reports, 37 prospective studies, 8 retrospective studies.
Major adverse events
- Osteomyelitis and protothecosis; 1 fatal necrotizing fasiitis; cellulitis and ecchymosis; tendon ruptures; atrophy of the plantar fat (after injecting neuroma); local skin effects appeared as atrophy, hypopigmentation of as skin defect.
Minor adverse events
Skin rash, flushing, disturbed menstrual pattern.
Increase pain or steroid flare after injection (19 studies)
After extra-articular injection the incidence of major adverse events ranged from 0-5.8%
Incidence of minor adverse events was 0-81%.
Overall, the reported adverse events were relatively mild, although 1 fatal reaction was reported.
Updated: Dec 31, 2018

